PCOS – What you should know
As a fertility doctor, I see women who are troubled by Polycystic ovary syndrome (PCOS) on a daily basis. Most of them come to see me because they have difficulty in trying to conceive and some of them have irregular menses, but many of them are unaware of their condition. Polycystic ovary syndrome (PCOS) is a relatively common health problem, affecting an estimated 1 out of 10 women of childbearing age. However, many women who come to see me are either unaware or misinformed about PCOS. To help dispel some of the misconceptions about PCOS, in today’s blog I’ll be explaining what PCOS is, what causes it and how it can be treated.
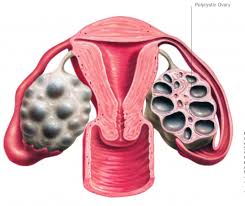
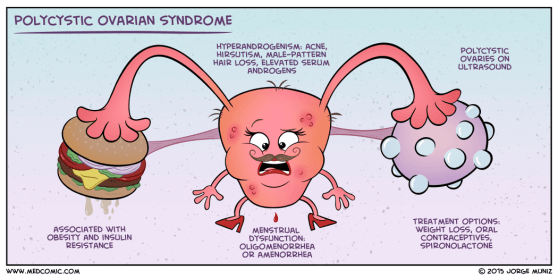
What is PCOS?
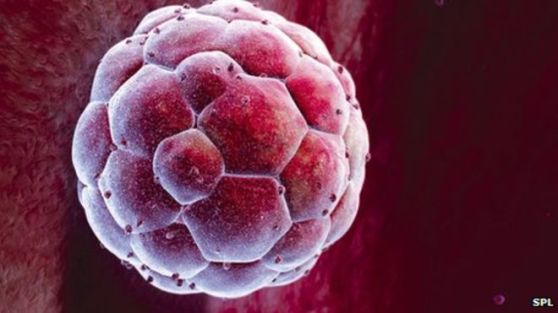
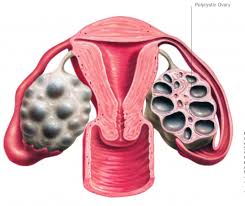
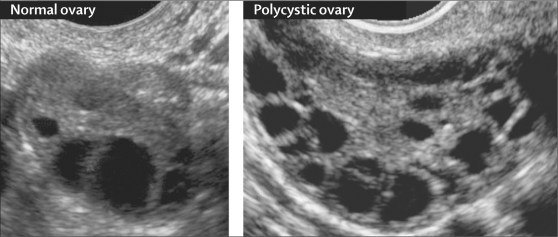
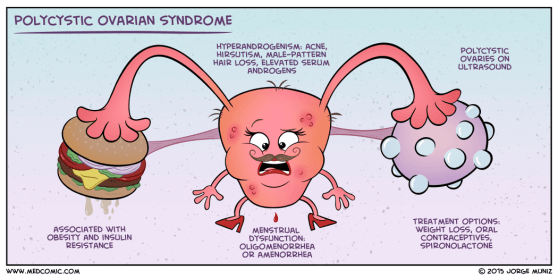
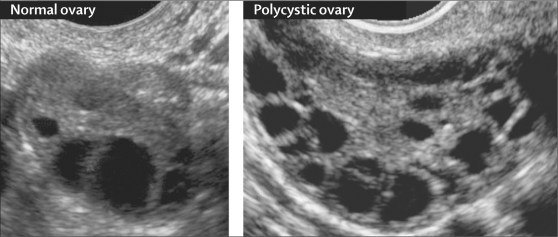
PCOS is a condition whereby small ‘cysts’ develop on a woman’s ovaries. In actual fact, these ‘cysts’ are not actually cysts per se, but are ovarian follicles which contain eggs. A healthy young woman will usually have about 5-10 follicles in each ovary, however, in the case of PCOS, each of the ovaries contain more than 10-12 follicles. Although these follicles are a sign of abundance in egg numbers, they cause the body to have hormone imbalances. Because hormones are chemical messengers, responsible for triggering various different processes in our bodies, when a hormone imbalance occurs it causes detrimental chain reactions.
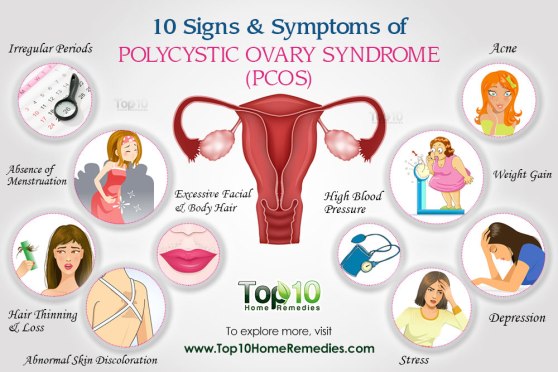
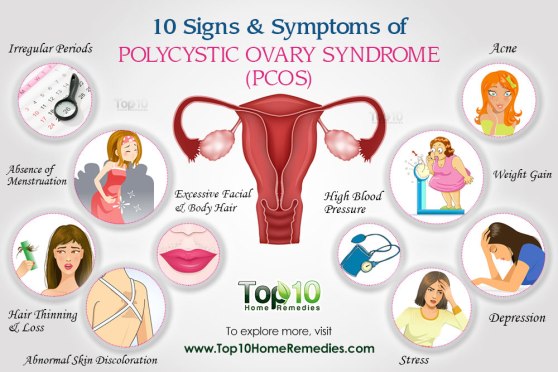
For example, PCOS can cause the ovaries to produce more androgens (male sex hormones), which disrupts ovulation, causes irregular periods, as well as causes acne and extra body or facial hair. PCOS can also cause insulin resistance, which increases blood sugar levels and can cause diabetes over time.
Other health issues caused by PCOS are metabolism problems, heart disease and infertility. If you have a family history of PCOS, on either your mother or father’s side, your chance of getting it is much higher.
PCOS Symptoms
Most women with PCOS share a number of common symptoms such as weight gain or trouble losing weight; extra facial or body hair (especially on the face, chest, belly and back); hair thinning on the scalp; irregular, few or no periods; heavy periods; fertility problems and depression. You may have many or just a few of these symptoms.
Diagnosis
In order to diagnose PCOS, your doctor will begin by asking you a series of questions about your health, symptoms and menstrual cycles. This will be followed by a physical exam, which will look for excessive body hair and high blood pressure, as well as take note of your body mass index (BMI). Next, some of your blood will be drawn to test your blood sugar, insulin and other hormone levels. Finally, you may have a pelvic ultrasound to look for cysts on your ovaries. Early diagnosis and treatment is crucial, as it can help you to control the unpleasant symptoms of PCOS, as well as prevent long-term health problems.
Treatment
Positive lifestyle changes can have a profound effect in treating PCOS. They not only reduce the unpleasant symptoms that you may experience, but also help prevent long-term health issues. To kick start your PCOS treatment, fit in moderate to vigorous exercises to your daily routine, such as walking, swimming, aerobic dancing and bicycling.
You should also eat a healthier diet, comprising of lots of vegetables, fruits, nuts, beans and whole grains. You should also reduce your intake of high calorie food which are high in saturated fat and carbohydrate. These life style changes will improve your weight and reduces insulin resistance. If you are a smoker, quite smoking as it causes you to have higher androgen levels. Most polycystic women will also benefit from weight loss, which can help balance out your hormones and regulate your ovulation and menstrual cycle.
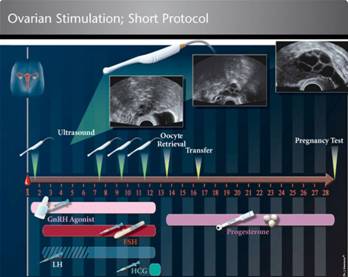
In addition to lifestyle changes, your doctor may prescribe you with medication to help reduce any symptoms you might be suffering, as well as to help you get pregnant. The common medications are ovulation inductions drugs, such as Clomiphene Citrate (Clomid) or FSH hormones injections. This will help you to ovulate naturally and increase your chance of pregnancy. Your doctor may also prescribe Metformin, which is a medication to reduce insulin resistance. This in turn will help to reduce weight, increase natural ovulations and reduces the androgenic effects of PCOS.
Laparoscopic ovarian drilling was once a popular surgery in reducing the effect of high androgens in PCOS patients. However, recent studies revealed that the effect of laparoscopic ovarian drilling is short-lived, i.e. the menstrual irregularity returns after a few months. On top of that, laparoscopic ovarian drillings has other adverse effects on women’s fertility, such as premature ovarian failure, adhesion formations causing tubal obstructions etc. Laparoscopic ovarian drilling is invasive and expensive especially in private settings. Therefore, it has become difficult to justify its cost against its effectiveness.

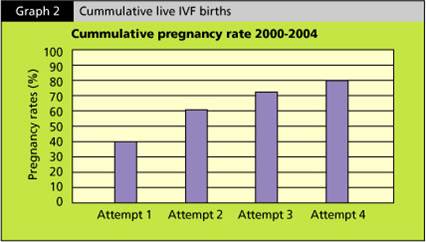
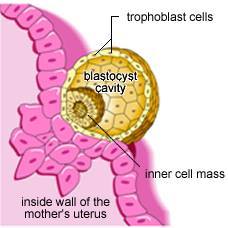
In some women, whereby there are other associated problems such as tubal obstructions or husbands’ sperms are weak or low in numbers, an IVF (In-vitro Fertilisation) treatment may be necessary and cost effective to achieve a pregnancy
Should you have any questions or concerns about PCOS and how it is affecting your health and chances of conceiving, as always, don’t hesitate to speak to your fertility consultant.
 sai
sai















 When it comes to family planning, women bear a disproportionate amount of the responsibility. There are very few male methods for family planning that are both practical and effective. Consultant obstetrician and gynaecologist Dr Helena Lim explores what’s on the horizon for safer and better family planning methods.
When it comes to family planning, women bear a disproportionate amount of the responsibility. There are very few male methods for family planning that are both practical and effective. Consultant obstetrician and gynaecologist Dr Helena Lim explores what’s on the horizon for safer and better family planning methods.